Health Alert: Novel Coronavirus (COVID-19)
COVID Testing Locations and updates for latest Queensland Government Information
Capsule endoscopy in the diagnosis of small intestinal pathology
Mark W A Norrie BHB, MBChB, FRACP, PhD
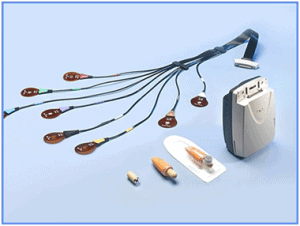
Capsule with Sensor array
 Since its introduction in 2000, capsule endoscopy has allowed us to investigate and diagnose pathology in the small intestine, a previously arcane area of the gastrointestinal tract.
Since its introduction in 2000, capsule endoscopy has allowed us to investigate and diagnose pathology in the small intestine, a previously arcane area of the gastrointestinal tract.
Presently it is funded by Medicare to investigate overt GI bleeding or occult bleeding with iron deficiency anaemia where a source has not been disclosed after gastroscopy and colonoscopy or for the surveillance of PeutzJeghers syndrome.
The procedure requires the patient to fast overnight and then swallow a capsule equipped with a light source and camera that tumbles through the small intestine and transmits two images per second to a recording device worn by the patient over an 8 hour time period. There is no anaesthetic involved, nor does the patient need to remain within the facility during this time thus ensuring minimal disruption. . The capsule is excreted normally with defaecation
The only significant risk with this procedure is capsule retention that occurs in about 1% of cases that may require surgical or endoscopic removal. This rate is higher (up to 8%) in patients with Crohns disease. In patients with a swallowing disorder, the capsule may need to be placed with a gastroscopy
 Capsule endoscopy has a sensitivity of 47% and 66.6% respectively for the detection of pathology in occult bleeding or iron deficiency anaemia. Where pathology is detected, the patient may then need to be referred for enteroscopy to obtain a tissue diagnosis or for interventional procedures.
Capsule endoscopy has a sensitivity of 47% and 66.6% respectively for the detection of pathology in occult bleeding or iron deficiency anaemia. Where pathology is detected, the patient may then need to be referred for enteroscopy to obtain a tissue diagnosis or for interventional procedures.
The most commonly diagnosed conditions include small bowel tumours in 5-7% cases as well as Crohns disease, NSAID injury and angioectasia.
Capsule endoscopy is available at Montserrat Day hospitals at our Indooroopilly facility and can be performed after the patient has had an antecedent gastroscopy and colonoscopy and following a brief consultation
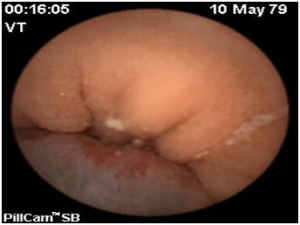
Small bowel tumour that presented with severe iron deficiency anaemia in a 27 year old male


